Konference: 2013 18th Congress of the European Hematology Association - účast ČR
Kategorie: Maligní lymfomy a leukémie
Téma: Chronic myeloid leukemia - Clinical
Číslo abstraktu: P150
Autoři: Prof. MUDr. Zdeněk Ráčil, Ph.D.; Ing. Filip Rázga, Ph.D.; Mgr. Jana Drápalová; RNDr. Lucie Burešová (Komolíková); MUDr. Daniela Žáčková, Ph.D.; MUDr. Martina Palacková; MUDr. Lukáš Semerád; MUDr. Lenka Malásková; Prof. Martin Haluzík, DrSc.; prof. MUDr. Jiří Mayer, CSc.
Background:
Hyperglycemia represents frequent adverse event reported in chronic myelogenous leukemia (CML) patients treated with nilotinib.
Aims:
To determine the major mechanism of glucose metabolism impairment, we performed a metabolic analysis using an oral glucose tolerance test as well as assessment of incretins and adipokines at baseline and after 3 months of nilotinib treatment in patients with CML.
Results:
10 patients were included in our study. 40% received nilotinib as first line, and 60% as second or subsequent line. 50% of patients received 600 mg and 50% received 800 mg of nilotinib/day. The median nilotinib Ctrough was 1510 (411-2973) ng/ml, median BMI was 27.2 (23.4-32.7) kg/m2, and median waist circumference was 93.5 (77.0-108.0) cm. Fasting, 1-, and 2-hour plasma glucose concentrations obtained during the OGTT significantly increased after 3 months of nilotinib therapy (Table). 2 patients fulfilled criteria of DM and 2 displayed IGT based on the OGTT. Nilotinib administration significantly increased fasting insulinaemia (Table 1).
Table 1.
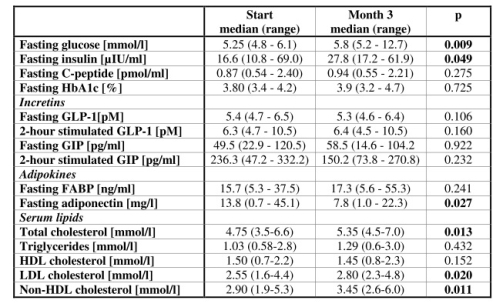
Moreover, there was also a trend of higher postprandial insulinaemia obtained during OGTT at the 3rd month of treatment (Table 1). C-peptide concentrations (fasting and during OGTT) and fasting HbA1C did not significantly change (Table 1). Insulin resistance as calculated by HOMA2-IR, significantly increased during nilotinib therapy (P=0.008). Moreover, the derived insulin sensitivity index HOMA2
Summary / Conclusion:
We proved that rapid insulin resistance, compensatory hyperinsulinaemia, and hypoadiponectinaemia develop after initiation of nilotinib therapy, which clarifies not only the mechanism of impaired glucose metabolism, but also at least partially explains the fast development of dyslipidaemia and peripheral artery occlusion in nilotinib-treated CML patients.
Datum přednesení příspěvku: 14. 6. 2013





