Konference: 2007 49th ASH Annual Meeting - účast ČR
Kategorie: Maligní lymfomy a leukémie
Téma: Postery
Číslo abstraktu: 1843
Autoři: MD Gertjan (J.L.) Kaspers, PhD; Martin Zimmermann, Ph.D.; MD Dirk Reinhardt, PhD; Rienk Tamminga; Brenda Gibson; Hortensia Armendariz; Prof. MD Michael Dworzak; S. Ha; Prof. Liisa Hovi; Alexei Maschan; N. Philippe; Bassem Razzouk; Carmelo Rizzari; MUDr. Petr Smíšek; Owen Smith; MD Batia Stark; A. Will; MD Ursula Creutzig, PhD
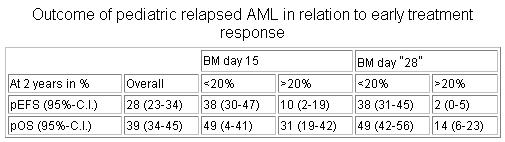
Taking duration of CR1 into account, patients with early relapse and BM blasts at day 28 of <20% had a comparable survival to those with late relapse and day 28 blasts of <20% (2-yr pOS 44% (34-55%) vs 53% (43-63%), p=.11). The survival of patients with BM blasts at day 28 20% was poor for both early and late relapses (2-yr pOS 11% (1-21%) vs 21% (3-39%), p=.08). In a Cox regression analysis of survival, BM day 15 lost statistical significance (p=0.27), while BM blasts day 28 20% (risk ratio 2.8, 95%-C.I. 1.7-4.7, p<.001) and early relapse (RR 1.52, 95%-C.I. 1.03-2.3, p=0.03) were each predictive for poor outcome after relapse. In conclusion, early treatment response is a strong and independent prognostic factor. A good early treatment response as determined on day 28 predicts a relatively favorable outcome in both early and late relapsed AML. Based on the day 28 bone marrow, patients that are very unlikely to be cured can be identified. These patients may be offered more experimental treatment. Alternatively, early treatment response may be useful for risk-group adapted therapy in relapsed AML.
Abstract #1843 appears in Blood, Volume 110, issue 11, November 16,
2007
Keywords: Bone Marrow|Risk Factor|Minimal Residual Disease
(MRD)
Disclosure: No relevant conflicts of interest to declare.
Sunday, December 9, 2007 6:00 PM
Session Info: Poster Session: Acute Myeloid Leukemias: Therapy,
excluding Transplantation II (6:00 p.m.-8:00 p.m.)
Datum přednesení příspěvku: 9. 12. 2007





