Konference: 2013 18th Congress of the European Hematology Association - účast ČR
Kategorie: Myelodysplastický syndrom
Téma: Myelodysplastic syndromes - Clinical
Číslo abstraktu: P194
Autoři: Anna M. Aalbers; MD Marry M. van den Heuvel-Eibrink, PhD; MD Valerie de Haas, Ph.D.; Jeroen G. te Marvelde; A. de Jong; Mirjam van der Burg; Prof. MD Michael Dworzak; Prof. MD Henrik Hasle; Prof. MD Franco Locatelli, PhD; MD Barbara De Moerloose; MD Markus Schmugge (Schmugge-Liner); prof. MUDr. Jan Starý, DrSc.; MD Marco Zecca; MD Christian Michel Zwaan, PhD; M.D. Arjan A. van de Loosdrecht, Ph.D.; MD Jacques J.M. van Dongen, PhD; Prof. MD Charlotte M. Niemeyer, PhD; Vincent H.J. Van der Velden, PhD
Background:
Refractory cytopenia of childhood (RCC), defined as myelodysplasia without an increased blast count, is the most common subtype of childhood myelodysplastic syndrome (MDS). Karyotype is normal in the majority of patients with RCC, and, in contrast to adults with MDS-refractory anemia (RA), about 80% of children have a hypocellular bone marrow. Although morphologic criteria for diagnosing RCC are strictly defined, differentiating RCC from the immune mediated bone marrow failure syndrome aplastic anemia can be challenging. Flow cytometry immunophenotyping has been suggested to be a valuable addition to morphology in the diagnosis of MDS in adults. Recently, a reproducible flow cytometry scoring system has been described as diagnostic tool by Ogata and others in adult low-grade MDS, with a sensitivity of 70% and a specificity of 93% (Ogata et al. Haematologica 2009 and Della Porta et al. Haematologica 2012).
Aims:
We investigated whether the flow cytometry scoring system described by Ogata and others is applicable in childhood MDS, with emphasis on RCC.
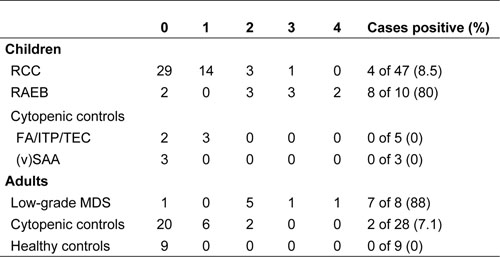
Table 1.
Methods:
Bone marrow samples, obtained from 82 previously untreated primary RCC patients, who were included in the prospective studies EWOGMDS 2006 and EWOG-MDS RC06 and diagnosed between June 2005 and December 2011, were analyzed by flow cytometry. Diagnosis of RCC was based on WHO criteria for pediatric MDS and confirmed by central review of bone marrow morphology and histology. Pediatric MDS-RAEB or RAEB-t patients, low-grade adult MDS patients, healthy individuals, and cytopenic non-MDS adult and pediatric patients were used as controls. Samples were evaluated based on the published criteria and cut-offs: CD34+ myeloid blast cells (parameter 1) ≥2%, CD34+ B-cell progenitors within CD34+ blast cells (parameter 2) ≤5%, lymphocyte/myeloid blast cell CD45 MFI ratio (parameter 3) ≤4 or ≥7.5, granulocyte/lymphocyte SSC peak channel ratio (parameter 4) ≤6. Patients scored 1 point for each fulfilled criteria; patients scoring 2 or more points were considered likely to have MDS.
Results:
The median age of included RCC patients was 10.5 years (range: 1-18 years). Bone marrow was hypocellular in 81% of patients; cytogenetic analysis was normal in 76% of patients, monosomy 7 was present in 6%, and other cytogenetic aberrations in 6%. In 35 of 82 patients (43%), insufficient blast cells and/or granulocytes were present for reliable analysis of all four parameters. Of the patients who could be evaluated completely, 4 of 47 patients (8.5%) scored ≥2 points, and were thus likely to have MDS according to the previously published criteria. The patients who scored positive were slightly older than the total RCC cohort (median age at diagnosis: 13 years); 2 patients carried a monosomy7, and in 2 patients no cytogenetic result was obtained due to insufficient metaphases. Results obtained in evaluable RCC patients and controls are summarized in Table 1.
Summary / Conclusion:
The scoring system proposed by Ogata and others is not usefully applicable in RCC due to a limited number of patients that can be evaluated for all four parameters, and due to a low sensitivity in those patients that can be evaluated. To evaluate whether other immunophenotypic abnormalities are present and might aid in diagnosing RCC, more detailed analyses of myeloid maturation patterns are currently underway.
Datum přednesení příspěvku: 14. 6. 2013





